Many men assume that feeling tired, gaining weight, or losing interest in sex is just part of getting older.
But these changes may be symptoms of a condition few men talk about—and even fewer understand.
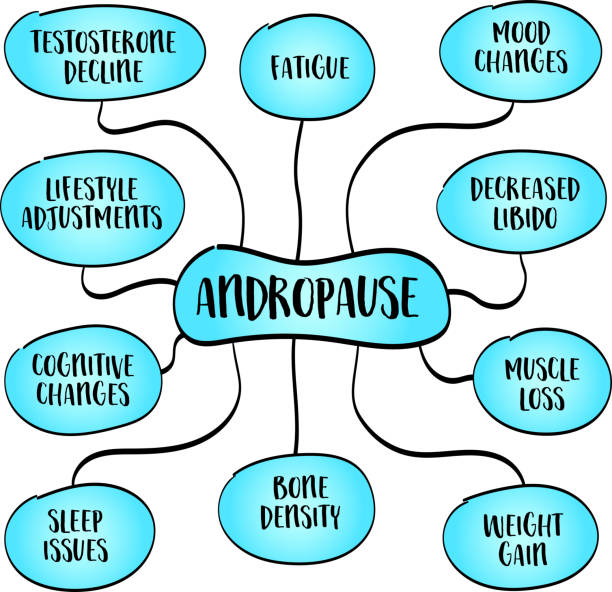
Andropause, sometimes called male menopause, refers to the natural decline in testosterone that typically begins between ages 40 and 55.
This hormonal shift, medically known as hypogonadism, affects an estimated 13 million men in the United States and can begin earlier due to stress, poor sleep, lack of exercise, or poor diet.
Unlike the sudden hormonal changes women experience during menopause, andropause unfolds gradually.
Because of that, many men don’t realize their symptoms—fatigue, low libido, mood changes, or reduced muscle mass—may be linked to low testosterone levels rather than just the aging process.
Testosterone is a critical hormone responsible for regulating energy, mood, sexual health, bone density, and muscle development.
As levels decline, men may find themselves feeling less focused, less motivated, and less resilient.
According to a review published by the Mayo Clinic,
Testosterone levels begin to drop by about one percent per year after age 30, and this decline can accelerate under chronic stress or unhealthy lifestyle conditions.
When testosterone dips below a healthy threshold, it can significantly impact both mental and physical well-being.
Common symptoms include decreased muscle mass and strength, erectile difficulties, low energy, increased body fat, and even mild depression.
Some men report sleep disturbances or reduced concentration, which can affect work performance and relationships.
The psychological impact is often underestimated.
Low testosterone is strongly associated with decreased motivation, irritability, and even clinical depression in some cases, as highlighted by research from the Journal of Clinical Endocrinology & Metabolism.
Because these symptoms can overlap with other conditions or be brushed off as signs of aging, andropause is frequently overlooked or misdiagnosed.
Fortunately, low testosterone is treatable—and recognizing the signs is the first step toward improvement.
Lifestyle plays a central role in managing andropause.
Diet, physical activity, stress management, and sleep quality can all influence hormone levels.
In fact, a study published in Nature Reviews Endocrinology found that weight loss, resistance training, and reducing sugar intake significantly improved testosterone levels in men with early signs of hypogonadism.
For men experiencing symptoms, a hormone test can confirm whether testosterone levels are in a healthy range.
From there, a doctor can help develop a personalized plan, which may include lifestyle modifications, supplementation, or medically supervised testosterone replacement therapy if appropriate.
It’s important to work with a trusted healthcare provider to understand the risks and benefits of any treatment.
Left unaddressed, low testosterone can lead to long-term health consequences, including reduced bone density, heart disease risk, and ongoing cognitive decline.
Yet with proper care, most men see meaningful improvements in energy, mood, and quality of life.
Andropause is not a weakness or failure—it is a natural biological transition.
The good news is that men no longer have to suffer in silence or guess what’s going wrong.
Science now offers clear answers and actionable solutions.
If you recognize some of these symptoms in your own life, consider reaching out for a consultation.
With knowledge, support, and the right care, you can restore balance and vitality for the years ahead.
Aging is inevitable.
But how you age is up to you.
